Abstract
Background
SCD is a chronic debilitating disease secondary to frequent veno-occlusive events resulting in chronic organ damage, including cerebral vasculopathy, acute chest syndrome (ACS), pulmonary hypertension and a significantly shortened life-span (Bunn et al, NEJM, 1997; Lanzkron et al, PHR, 2013; Platt et al, NEJM, 1994). Importantly, SCD survivors also develop significant defects in neurocognition, especially processing speed and have a poor HRQL (Stotesbury et al, Neurology, 2018); Vichinsky et al, JAMA, 2010; Panepinto et al, BJH, 2005). To date the only cure for SCD patients has been HLA matched sibling AlloSCT following either myeloablative (MAC) or reduced toxicity conditioning (RTC), (Walters et al, NEJM, 1996; Bhatia/Cairo et al, BMT, 2014; Talano/Cairo et al, EJH, 2015; Gluckman et al, Blood, 2017). Unfortunately, only approximately 15% of patients have an unaffected HLA matched sibling donor (Mentzer et al, AJPHO, 1994). We previously demonstrated the safety and efficacy of CD34 enrichment and mononuclear cell (MNC) addback (2 x 105 CD3/kg) in pediatric matched unrelated donor recipients (Geyer/Cairo et al, BJH, 2012). We now report the long term results of MAC and familial HISCT utilizing CD34 enrichment and MNC (CD3) addback in high risk SCD recipients.
Methods
SCD patients with one or more high risk features (cerebral vasculopathy, repetitive ACS, repetitive VOC, abnormal TCD requiring RBC TX) underwent MAC and parental HISCT consisting of hydroxyurea, azathioprine, fludarabine, busulfan, cyclophosphamide, thiotepa, r-ATG and TLI and PBSCT utilizing CD34 enrichment (10x106 CD34/kg) (Miltenyi®) and MNC addback (2x105 CD3/kg) and tacrolimus AGVHD prophylaxis x 100 days as we have previously described (Talano/Cairo et al, ASH, 2017). Donor chimerism in WBC and RBC (CD71) enriched fractions was determined centrally as we have previously described (Geyer/Cairo et al, BJH, 2012). AGVHD & CGVHD were determined utilizing the Glucksberg and NIH consensus criteria, respectively. Transthoracic echocardiogram, TRJ velocity, PFTs, MRI/MRA were performed at baseline and 2 years. Neurocognitive testing utilizing DIVERGT screening was performed at baseline and 2 years as we have previously described (Vichinsky et al, JAMA, 2010; Krull et al, JCO, 2008). HRQL testing utilized the CHRIS-General and CHRIs-HSCT (age appropriate) at baseline and Days +45, 100, 180, 365 and 730 post HISCT as we have previously described (Kelly/Parsons et al, PBC, 2012).
Results
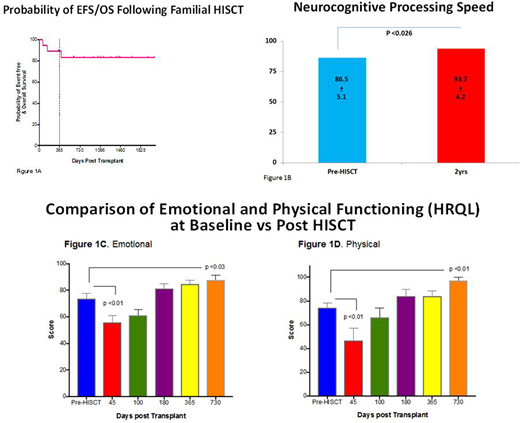
Among the 19 HISCT recipients, the mean±SEM age was 13.1±1.2 years (3.3-20.0) years, gender 12/7 (M/F). There were 18 parental haploidentical donors with mean±SEM age of 41.3±1.8 (30-55) years, gender 15/3 (F/M). The mean±SEM CD34 enriched PBSC infused was 10.94±0.4x106/kg and MNC addback (2 x 105 CD3/kg). The median time to neutrophil and platelet engraftment was day +9 and +19, respectively. The 1yr mean±SEM whole WBC and RBC (CD71) mixed donor chimerism was 97.1±1.4 and 96.4±2.0%, respectively. The cumulative incidence of grade II-IV AGVHD and CGVHD was 6.2% and 6.7%, respectively (Figure 1A). The probability of 1yr EFS was 90% (CI95 64-97%). In comparison from baseline to 2yr post HISCT, PFTs were stable to improved with a significant improvement in conductance (sGAW) (p<0.026), cardiac SF and TRJ velocity were stable to improved, MRI/MRA showed no new overt and/or silent strokes and no new cerebral vasculopathy. Intellectual functioning, memory, language, and executive function were also stable to improved. Most importantly, processing speed was significantly improved (p<0.026) (Figure 1B), emotional functioning (HRQL) (p<0.03) (Figure 1C) and physical functioning (HRQL) (p<0.01) (Figure 1D) were significantly improved at 2 years vs. pre-HISCT.
Conclusion
MAC and familial HISCT utilizing parental donors and CD34 enrichment and MNC addback (2 x 105 CD3/kg) in high risk patients with SCD was well tolerated, resulted in rapid hematological reconstitution, long term stable WBC and RBC (CD71) donor chimerism, low cumulative incidence of A+CGVHD and stable to improved pulmonary and cardiac function. There was also a significant improvement in processing speed and emotional and physical HRQL 2yrs post HISCT. This study was registered at clinicaltrials.gov (NCT02675959) and conducted under IND (14359) (MSC) and supported in large part by FDA R01FD004090.
Cairo:Janssen: Research Funding. Parsons:Seattle Genetics: Research Funding. Friedman:MedImmune/AstraZeneca: Consultancy, Speakers Bureau. Vichinsky:Global Blood Therapeutics: Consultancy, Honoraria, Membership on an entity's Board of Directors or advisory committees, Research Funding; bluebird bio: Membership on an entity's Board of Directors or advisory committees; Protagonist: Research Funding. Walters:Sangamo Therapeutics: Consultancy; bluebird bio: Research Funding; ViaCord Processing Lab: Other: Medical Director; AllCells Inc.: Other: Medical Director. Shenoy:Novartis, Vertex, Bluebird Bio: Honoraria, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal